Protocols Assist with Improving Communication for Patients with Tracheostomy & Ventilator Dependence
Carmin Bartow, MS, CCC-SLP, BCS-S | Meredith Oakey Ashford, MS, CCC-SLP

Introduction
For patients with tracheostomy and ventilator dependence, communication in the intensive care unit can be difficult to achieve but having a reliable means of communication is imperative for health, safety, and well-being. The Speech-Language Pathology (SLP) team at Vanderbilt University Medical Center (VUMC) recently launched a six-month quality improvement initiative to promote early intervention for this patient population. The project, “Improving Communication for Patients with Tracheostomy and Ventilator Dependence,” had a primary goal of establishing consistency with communication for these patients by having the entire SLP department trained in a newly developed protocol. Prior to this project, only some of the SLPs in the department were fully confident and competent in providing intervention to these patients. With the development and implementation of this program, patients may participate more readily in their medical plan, which can improve efficiency of care by all staff, preventing unnecessary delays in their care, which may have occurred secondary to the earlier difficulties with communication and patient participation.
Purpose
Impaired communication can lead to safety concerns, violation of patient rights, poor quality of life, and may contribute to ICU delirium (Freeman-Sanderson, Togher, Elkins, & Kenny, 2018). Some of the reasons for addressing communication are:
- Safety concerns: Patients with communication problems were three times more likely to experience preventable adverse events than patients without such problems (Bartlett, Blais, Tamblyn, Clermont, & MacGibbon, 2008). Serious medical events have been reported for patients with impaired communication (Cohen, Rivara, Marcuse, McPhillips, & Davis, 2005).
- Patient rights: The Joint Commission set new standards which focus on all patients having their communication needs met, making communication a priority. The Joint Commission upholds that patients have a “right and need to effective communication.” In the Elements of Performance for R1.2.100, No. 4 states, “The organization addresses the needs of those with vision, speech, hearing, language, and cognitive impairments” (The Joint Commission, 2010).
- Quality of life: Inability of the ICU patient to communicate can lead to frustration, anger, withdrawal from interaction, and reduced participation in treatment (Magnus & Turkington, 2006).
- ICU Delirium: Two out of three patients in ICUs experience delirium (Grossbach, Stranberg, & Chlan, 2011). In a Joint Commission webinar, Call to Action: Improving Care to Communication Vulnerable Patients, it was reported that communication-vulnerable patients have an increased diagnosis of psychopathology (The Joint Commission, n.d.).
- The Vanderbilt Promise: “As an institution, VUMC promises to include you [the patient] as the most important member of your healthcare team” and “communicate clearly and regularly, which is paramount during times of critical illness.”
Implementation Methods and Communication Access
To improve the consistency and standardization of assessment and treatment for the patient with tracheostomy and ventilator dependence, the SLP team members who were competent with this patient population:
- Developed a protocol to standardize assessment of both verbal and non-verbal communication.
- This protocol starts with a readiness screening. If the patient passes the screening, it then provides a workflow for a collaboration between the speech-language pathologist and the respiratory therapist (RT) during phonation trials.
- Collaboration would involve basic assessment of speech, language, and cognition and the need for a simple AAC (Augmentative and Alternative Communication) tool.
- Disseminated this protocol to the acute speech pathology staff through didactic teaching, oneon-one training, and competency check offs.
- Met with the Director of the VUMC Critical Illness, Brain Dysfunction, and Survivorship Center to discuss the importance of communication for patients following tracheostomy and mechanical ventilation to potentially minimize delirium.
- Provided in-services to the interprofessional disciplines that collaborate on the care for these patients, including:
- Respiratory therapists.
- Medical Intensive Care Units (MICU) attendings and fellows (physicians).
- Nursing staff throughout VUMC.
- Created a poster presentation for a hospital-wide Strategy Share Program in order to further disseminate the improvement process. The theme for the 2019 Strategy Share was “Design for Patients and Families.” This CQI project fit perfectly with this theme and the VUMC goals of enhanced patient, clinician, and staff experiences.
Results
This qualitative process and review of its impact provided a means of training personnel and reviewing the impact on staff confidence and workflow. Review of interview data demonstrated that implementing the improvement process through additional training increased the confidence of the SLP team when serving this population. After the departmental in-service trainings, SLPs commented:
- “The in-service enabled me to gain skills and confidence to feel more prepared to treat these complex patients.”
- “I feel better equipped to manage our trach/ vent patients.”
Furthermore, respiratory therapists and speech-language pathologists demonstrated improved teamwork to establish communication for these patients. A pre-project staff survey was completed to ascertain staff comfort and efficiency when treating these patients. A post-training survey is in process. Preliminary results indicate that staff has the improved confidence, knowledge, and skills to work with these complex patients.
In addition to improvement in patient care, the SLP team also benefitted from this initiative by receiving increased recognition within the medical center. The poster, which provided education on the protocol for working with patients to enhance communication, was well-received at the VUMC Strategy Share event. This initiative also led to an invitation for the SLP team to participate in the VUMC Critical Illness, Brain Dysfunction, and Survivorship Center.
Most importantly, the patients who have benefited from this program consistently report appreciation for being able to express themselves and actively participate in their care. One patient stated, “It has been so frustrating trying to tell my husband what I want. He couldn’t read my lips so I tried to write, but he couldn’t read my writing. Now, I can just talk to him, and it’s so much better.”
Conclusions
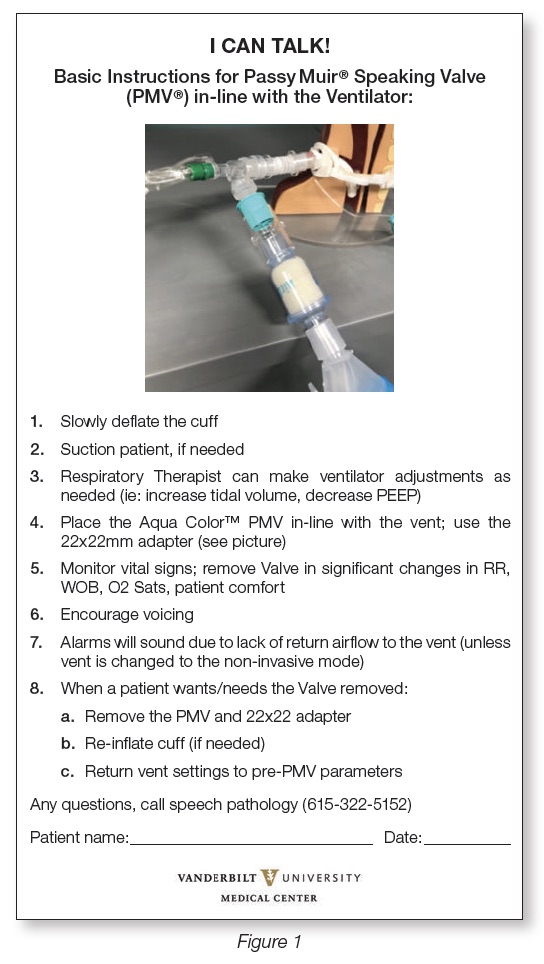
In collaboration with physicians, ICU nurses, the Trach Consult Service, and respiratory therapists, the Adult Acute Speech-Language Pathology team is making verbal and non-verbal communication accessible for these otherwise non-communicative patients. Hospital staff will now interact more efficiently with patients from this intervention by using the newly implemented head-of-bed sign, directing them on how to facilitate verbal communication with their patient (see Figure 1). This simple form improves consistency in communication across the interdisciplinary team for these vulnerable patients. Improving communication with this population has resulted in improved safety, quality of life, and compliance with Joint Commission regulations, ADA laws, and the VUMC Patient Promise.
This article is from the Fall 2019 Protocol Issue of Aerodigestive Health. Click here to view Protocols Assist with Improving Communication for Patients with Tracheostomy & Ventilator Dependence.
References
Bartlett, G., Blais, R., Tamblyn, R., Clermont, R. J., & MacGibbon, B. (2008). Impact of patient communication problems on the risk of preventable adverse events in acute care settings. Canadian Medical Association Journal, 178, 1555-1562. doi: 10.1503/cmaj.070690
Cohen, A. L., Rivara, F., Marcuse, E. K., McPhillips, H., & Davis. R. (2005). Are language barriers associated with serious medical events in hospitalized pediatric patients? Pediatrics, 116(3),575-9.
Freeman-Sanderson, A. L., Togher, L., Elkins, M. R., & Kenny, B. (2018). Quality of life improves for tracheostomy patients with return of voice: A mixed methods evaluation of the patient experience across the care continuum. Intensive Critical Care Nursing, 46,10-16. doi:10.1016/j.iccn.2018.02.004
Grossbach, I., Stranberg, S., & Chlan, L. (2011). Promoting effective communication for patients receiving mechanical ventilation. Critical Care Nurse, 31(3): 46-61.
The Joint Commission. (2010). Advancing effective communication, cultural competence, and patient- and family-centered care: A roadmap for hospitals.[brochure]. Retrieved January 15, 2019 from https://www.jointcommission.org/ assets/1/6/ARoadmapforHospitalsfinalversion727.pdf
The Joint Commission. (n.d.). Call to Action: Improving care to communication vulnerable patient. [brochure]. Retrieved January 15, 2019 from http://www.patientprovidercommunication.org/files/CommunicationVulnerableWebinar.pdf
Magnus, V. & Turkington, L. (2006). Communication interaction in ICU-patient and staff experiences and perceptions. Intensive Critical Care Nursing, 22, 167-180.












